THE PSYCHOLOGY OF POLIO AS PRELUDE TO
POST-POLIO SEQUELAE:
Behavior modification and psychotherapy
Richard L. Bruno, Ph.D.¹ and Nancy M. Frick, M.Div.²
Bruno RL, Frick NM. The psychology of polio as prelude to Post-Polio
Sequelae: Behavior modification and psychotherapy. Orthopedics, 1991,
14(11) :1185-1193.
Lincolnshire Post-Polio Library copy by arrangement with the Harvest
Center Library
1. Post-Polio Rehabilitation and Research Service
Kessler Institute for Rehabilitation
East Orange, New Jersey
and
Department of Physical Medicine and Rehabilitation
New Jersey Medical School
University of Medicine and Dentistry of New Jersey
2. Harvest Center
Hackensack, New Jersey
Address correspondence to:
Nancy M. Frick, M.Div.,
Harvest Center,
151 Prospect Avenue,
Hackensack, New Jersey 07601
THE PSYCHOLOGY OF POLIO AS PRELUDE TO POST-POLIO SEQUELAE:
Behavior modification and psychotherapy.
Richard L. Bruno, Ph.D.¹ and Nancy M. Frick, M.Div.²
ABSTRACT
Even as the physical causes and treatments for Post-Polio Sequelae (PPS) are being
identified, psychological symptoms - chronic stress, anxiety, depression and
compulsive, Type A behavior - are becoming evident in polio survivors. Importantly,
these symptoms are not only themselves causing marked distress but also are preventing
patients from making the lifestyle changes necessary to treat their PPS. Neither
clinicians nor polio survivors have paid sufficient attention to the acute polio
experience, its conditioning of life-long patterns of behavior, its relationship to the

development of PPS and its effect on the ability of individuals to cope with and treat
their new symptoms. This paper describes the acute polio and post-polio experiences on
the basis of patient histories, relates the experience of polio to the development of
compulsive, Type A behavior, links these behaviors to the physical and psychological
symptoms reported in the National Post-Polio Surveys and presents a multimodal
behavioral approach to the treatment of PPS by describing patients who have been
treated by this Post-Polio Service.
ACKNOWLEDGEMENTS
The authors would like to thank those who have volunteered as research subjects and
our patients, whose experiences are the foundation of this report and who have allowed
themselves to be quoted for this paper. We would also like to thank Dr. Thomas Galski
for his criticism of the manuscript, Ms. Joan Kelly for her computer expertise and Mary
Ann Solimine, R.N., M.L.S., without whom this work would not have been possible.
This research was funded by grants from the Joel Leff and George Ohl Foundations.
THE PSYCHOLOGY OF POLIO AS PRELUDE TO POST-POLIO
SEQUELAE: Behavior modification and psychotherapy in treating PPS
Richard L. Bruno, Ph.D. and Nancy M. Frick, M.Div.
"I'll walk without crutches. I'll walk into a room without scaring everybody half to
death. I'll stand easily enough in front of people so that they'll forget I'm a cripple."
Franklin D. Roosevelt (1)
In the 1980's, nearly half of the 1.63 million American polio survivors reported new and
unexpected symptoms - fatigue, muscle weakness and pain - that have come to be called
Post-Polio Sequelae (PPS) (2,3). While the medical community focused its attention on
these new physical symptoms, polio survivors' psychological reactions to PPS emerged.
Fear, disbelief, denial and confusion were experienced first since PPS were completely
unexpected (4). The 1985 National Survey of 738 polio survivors (5,6) revealed that
86% of the respondents never considered the possibility of developing new problems
after having reached maximum recovery from polio and that 72% did not initially think
that their new symptoms were related to their having had polio. Since polio survivors
did not know the cause of their new symptoms they looked to the medical community
for help.
Fear and confusion increased as medical ignorance and disinterest frustrated and
angered polio survivors. Many physicians dismissed new symptoms as psychogenic,
factitious or unrelated to polio. In the 1985 National Survey, 23% of respondents were
told by physicians that the symptoms were "all in their minds" while 26% were told that
the symptoms "could not possibly be related to having had polio." Other patients
received frightening and unfounded diagnoses, such as "some kind of ALS" or
recrudescent polio (3). Many patients were told that they would have to accept new
symptoms and loss of function since all polio survivors were "just getting old" (4).

Now, in the second decade of PPS, the medical community has accepted the reality of
PPS and is identifying effective treatments for new fatigue, weakness and pain. Even
with these advances, additional psychological symptoms - chronic stress, anxiety,
depression and compulsive, Type A behavior - are being identified in polio survivors.
Importantly, these symptoms are not only themselves causing marked distress but also
are preventing patients from making the lifestyle changes necessary to treat their PPS
(6,7,8).
It appears that the factor central to the etiology of these psychological symptoms is that
polio survivors are being forced to cope with new symptoms and disability when many
have not yet dealt with the emotional reality of their having had polio over thirty years
ago. Evidence for the postponement of coping with the acute polio experience was
found in the 1985 National Survey, where 26% of respondents reported that they "did
not think of themselves as having a disability" before developing PPS; with the onset of
PPS 42% admitted to having a "second disability." (6)
Neither clinicians nor polio survivors have paid sufficient attention to the acute polio
experience, its conditioning of life-long patterns of behavior, its relationship to the
development of PPS and its effect on individuals' ability to cope with and treat their new
symptoms. It is the purpose of this paper 1) to describe the acute polio and post-polio
experiences on the basis of published reports and patient histories; 2) to relate the
experience of polio to the development of compulsive, Type A behavior; 3) to link
compulsive, Type A behavior to the physical and psychological symptoms reported in
the National Post-Polio Surveys; 4) to present a multimodal behavioral approach to the
treatment of PPS by describing patients who have been treated by this Post-Polio
Service during the past year.
The Acute Polio Experience
Polio survivors frequently report that the onset of PPS have forced them, often for the
first time, to recall and examine their acute polio experience (9). With the onset of polio,
these individuals understood that they had been stricken by the "greatly feared disease,"
believed that disability was likely and death was possible (10). These fears were
amplified in those who knew others who had been disabled or even killed by polio (10).
Polio survivors recall confusion and terror at being wrenched from their homes and
being given by their parents into the care of strangers with whom they were required to
live for weeks, months or even years (11). Even children too young to understand what
was happening likely sensed their parents' fear and panic; they certainly felt the pain of
their own illness and the desolation of being abandoned by their parents (11,12,13,14).
Individuals admitted to hospital quickly became aware of their complete loss of control
and total dependency on the hospital staff. Many could not feed or toilet themselves;
those with the most severe paralysis could not even move. Patients' were forced to rely
totally on hospital staff if their most basic survival needs were to be met. If they were to
survive, patients had little choice but to suppress their fears and follow their parents'
parting instruction: "Be good, don't make trouble and do everything you're told" (11).
Separation from parents and loss of control were not the only sources of fear. Patients
describe a hospital regimen of painful and often frightening therapies including hot
packs, splinting, bracing, stretching and exercise (15). Patients also report undergoing
multiple surgeries, including muscle transplants, tendon lengthenings and osteotomies.
One especially brutal procedure that many parents attempted to obtain for their children,
pulverized weakened muscles and their motor nerves with an electric riveter to promote
axonal sprouting - a uniquely medieval attempt to prevent permanent visible disability
(16,17). These procedures were administered usually without explanation and certainly
without consent since, especially at the height of the epidemics, hospitals were
overwhelmed by the sheer number of polio patients needing care
(10,11,12,13,15,18,19). Excluding young patients from treatment decisions and the
failure to communicate information about their illness magnified the severity of the
illness to the patients and permitted their inherent fear of death to emerge (14).
Questions or complaints about therapies were not infrequently met by staff anger or
punishment (13,18). Staff anger was viewed as a very real threat to survival by patients
who were isolated from parents and totally dependent on the staff. One patient described
this situation as placing her in "mortal danger" (15); she believed that the staff had to be
placated if she were to survive. Patients discovered that staff anger could sometimes be
prevented if they complied with hospital regimen without questions. Full participation
in therapies, without regard to pain or exhaustion, would sometimes garner brief
attention or even praise. Thus, the expression of personal needs and emotion were
punished by the staff while unquestioning compliance with and performance for the
staff were reinforced. Unfortunately, protection from punishment could not always be
assured. Patients describe staff who acted with unnecessary cruelty in maintaining order
and control on the ward. Family visits were restricted to only a few hours per week,
reinforcing patients' feelings of parental abandonment and dependency upon staff
(12,15,20). Normal, child-like behaviors were punished excessively. Several patients
reported having been locked in a completely dark closet overnight when they spoke or
cried after "lights out." Even appropriate and necessary nursing care could be withheld
for no apparent reason (15,18).
Many of the patients treated by this Service have related other instances of
psychological, physical and even sexual abuse at the hands of hospital staff. Instead of
causing patients to complain, such abuse further reinforced patients' belief that survival
depended upon the suppression of personal needs and emotion and unquestioning
compliance with those in authority. This belief is evidenced in one patient's rationale for
not reporting repeated sexual abuse: "I would have made my parents angry because I
was not doing what I was told and the nurses, who I depended on for everything, would
have punished me for making trouble for them. All I could do was stop feeling bad
about it and smile."
Under these circumstances, some patients report having lost their sense of "identity"
(18,20). Some report over-identifying with the staff and even expressed the desire to
become "orthopedic surgeons when they grew up" (21). Others apparently submitted so
completely to the hospital staff that they did not wish to go home or even asked to
return to the hospital following discharge (22,23). It appears that many polio survivors
learned to deal with their abandonment, loss of control, fear, pain and abuse by
submitting to those in authority, complying fully with external expectations and denying
personal needs, physical and emotional pain and even their own individuality (24).
These behaviors are evident in this summary of the "Good Chart" written by polio
wardmates at Baltimore's City Hospital (22):
LISTEN TO THE DOCTORS
OBEY THE NURSES
DO NOT FIGHT
DO NOT BE BAD
BE GOOD IN SCHOOL
DO YOUR HOMEWORK
DO NOT TALK AT DINNER or IN SCHOOL
LITTLE FOLKS SHOULD BE SEEN AND NOT HEARD
When polio patients returned home as "polio survivors," the "Good Chart" became their
prescription for proper behavior. They had learned very young and very well that
submission, compliance and suppression of emotion were required if they were to
escape "mortal danger"(15).
Polio Survivors in the Community
When polio survivors re-entered their communities, any special attention that may have
been provided to them and their families during the acute polio often quickly stopped
(22). Friends of polio survivors' families, unable to deal with the reality of polio, often
disappeared (22). It was not uncommon for neighborhood children to be prohibited from
playing with "polio victims" for fear that the "crippling" was contagious (23). Polio
survivors, no longer physically able to participate easily or fully in social activities,
became isolated (10,25). Such alienation and isolation made polio survivors pariahs
(10,14,22,25).
However, there was "hope." Individuals had been imbued with the "unqualified progress
ideology" of physical therapy following their acute illness and had often been given
prognoses upon discharge that were unrealistically optimistic (26). One paraplegic
woman was told, "You'll walk out of your braces before you start dating." Such
prognoses were seen as a call to normalcy. The use of braces, crutches and wheelchairs,
that had made mobility possible and had been symbols of triumph over paralysis in the
hospital, became stigmata of "the crippled" and symbols of one's failure to have
recovered completely. Necessary assistive devices were quickly discarded, regardless of
the discomfort, fatigue, awkwardness or pain that resulted, as individuals strove for the
"appearance of complete physical normalcy" (21,27). Painful and exhausting physical
therapies were resumed upon patients' return home from hospital or initiated in those
who were not hospitalized. Physical therapy often continued for more than a decade
after the acute polio with the only goal being "complete recovery" (11). One patient,
who became triplegic at age six and has consistently thereafter used a wheelchair,
continued daily physical therapy until she left home for college, "Everyone believed that
physical therapy would make me walk - eventually." As motivation to walk without
braces, another patient was repeatedly beaten by his father who said, "I'd rather see you
dead than a cripple."
The abuse of polio survivors by parents was usually less overt but was not infrequent,
being motivated by a denial of polio and revulsion by disability (13,14,27). Some polio
survivors report being physically trapped by their parents' refusal to make
accommodations for their physical limitations. Homes frequently remained inaccessible,
making activities of daily living impossible without assistance from parents - assistance
that could be inconsistently provided or consistently withheld (28). One patient was
regularly carried outside in the early morning, regardless of the weather, where she
remained until dark. Another patient reported that he was locked in a car with windows
closed in the heat of midsummer so that his family could tour Washington's then
inaccessible national monuments. Polio survivors learned that physical abilities needed
to be maximized if they were to survive in a "barrier-full" society.
Other parents strove to reincorporate the child into the family routine and "forget" about
polio by requiring children to equal or exceed the level of physical performance they
exhibited before their illness (11). One patient's family took up hiking when their
daughter returned home from the hospital, expecting her to "learn to keep up with the
others" in spite of crutches and braces. Patients also report that they were expected to
out-perform their peers academically. Several patients reported that they would be
severely punished if they received "anything less than an "A"." Such academic
expectations reinforced the premature adult-like behaviors that were described in
children who had been hospitalized following the acute polio (22).
Still other parents experienced both "shame and estrangement" at having been "singled
out" by polio (22). Unable to deny the reality of their childs' disability, they isolated the
family from society and severely restricted their child's physical activities (11,14,22).
One patient, who had a barely noticeable limp following polio at 18 months, was
prevented from leaving his yard or playing with other children until he attended high
school. Such isolation impaired the development of social relationships (25,29,30) and
parental shame of disability was learned by the child (14). Unfortunately, many patients
report that their parents have consistently refused through the years to discuss anything
having to do with the physical or emotional reality of the polio experience (14,20). An
attempt at discussion with one 45-year old patient's mother was stopped by the angry
statement, "It's all too painful for me. Don't ever mention it again."
Whether unrealistically demanding or overly restrictive, parents' powerful expectations,
combined with those of physicians, nurses and therapists, dictated the behaviors that
were required of polio survivors if they were to escape "mortal danger" (15) and be
accepted by parents and society. Yet, despite the fulfillment of these expectations by the
achievement of a remarkable degree of functional recovery in most individuals and even
the appearance of "normalcy" in many, polio survivors were told that they were still not
acceptable (31). They report being told by teachers that no one would ever hire them, by
parents that no one would ever marry them, and by physicians that they should never
have children (28,32,33). Thus, as polio survivors entered adulthood they had
internalized the expectations of those in authority, which led to self-alienation and
actual participation in the "execution of the self" (24). Polio survivors continued to
follow the prescription for proper behavior set forth in the "Good Chart" even though
they had been told that fulfilling the expectations of others would not result in
acceptance by society (34).
Type A Behavior as a Post-Polio Sequelae
The majority of polio survivors have succeeded in minimizing the appearance of
disability, maximizing independence and "disappearing" into society (28). Most polio
survivors have learned to walk after discarding nearly all of their original assistive
devices (6). Despite society's negative expectations, polio survivors have had more
years of formal education and a larger proportion of them are married as compared to
the general disabled and non-disabled populations (Table 1)(35). Polio survivors also
have a higher level of employment as compared to the general disabled population (36).
These data suggested the hypothesis that polio survivors have not merely achieved
"normalcy" but have actually surpassed it by learning physically and emotionally
stressful Type A behavior as a response to their experience of polio (5,28,37). The polio
experience should have provided an ideal environment for the conditioning of Type A
behavior. Type A behaviors are thought to learned in service of the "active avoidance of
punishment" (38) by individuals who are engaged in a chronic "struggle to overcome
environmental barriers" (39) "against the opposing efforts of other things or persons"
(40). Further, Powell, et al (41) found that a "consistent set of beliefs and attitudes about
the self, others, and life in general lay beneath the overt (Type A) behavior," including
"low social support," "low self-esteem" and loss of control. Such beliefs would be the
likely consequence of the above-described experience of polio.
To test the hypothesis that polio survivors are Type A, the Brief Type A Questionnaire
(42) was administered to 738 polio survivors as part of the 1985 National Post-Polio
Survey (5). Polio survivors' mean Type A score of 53±22 was significantly higher than
that of non-disabled controls (36±14). This finding was replicated by the 1990 National
Survey of 373 polio survivors (6) who had a significantly elevated mean Type A score
of 59±22 as compared to non-disabled controls (45±20) and adults with spina bifida
(48±22)(Table 2).
Since it had been suggested that Type A individuals are hypersensitive to criticism (41),
the 1990 National Survey also included the Reinforcement Motivation Survey (RMS)
(43) that contains a Sensitivity to Criticism and Failure Scale. Polio survivors had a
significantly elevated mean Sensitivity to Criticism and Failure score (68±28) as
compared to non-disabled controls (59±27) that was significantly correlated with the
Type A score (r=0.44)(5). This correlation suggests that Type A behavior in polio
survivors serves in part to prevent criticism and to protect against feelings of failure
(21,44).
Compulsive Behavior as a Post-Polio Sequelae
The majority of patients treated by this Service not only demonstrate Type A behavior
but also evidence behaviors that are not typically Type A. Patients describe an inability
to express emotion or admit having physical pain ("I can't complain because people
expect the handicapped to complain"). They inflexibly and punitively judge their own
behavior on the basis of what is "normal" and on unachievable ideals of perfection. One
patient stated, "If I fail at anything, I might as well die. It boils down to either using
every ounce of my energy to lead a normal, successful life or giving in to my
weaknesses and being inferior."
Patients also demonstrate a strong need to be in control (15) and report marked anxiety
with and nearly phobic avoidance of any change ("I am constantly moving and in a
constant state of fear. I feel if I slow down, I'll never get started again") or decrease in
the number or extent of their activities ("I can't just sit and do nothing"). These patients
refuse to slow down, delegate responsibilities or allow others to assist them even when
they experience fatigue, weakness and pain. They report a saw-tooth pattern of activity,
characterized by working until physical symptoms prevent them from continuing.
Exhausted, anxious and fearful of criticism, they rest until activity is again possible and
then work until symptoms force them to halt. As one polio survivor stated, "I have spent
my whole life pushing to keep going and I still push myself even though I know I
shouldn't. I keep going until I can no longer walk or stand the pain. I cannot be stopped.
I work until I fall."
Patients also report that they "must" satisfy the real or perceived needs of others ("I can't
ever say 'No'") and some describe a compulsion to perform nearly ritualistic behaviors
in order to escape "mortal danger" (15). One patient stated, "I know it's ridiculous, but I
believe that if I make the bed every day I'll never die; I will earn the right to continue to
live."
These behaviors are reminiscent of the Obsessive Compulsive Personality Disorder
(OCPD)(45). However, polio survivors' compulsive behavior differs from OCPD in
important ways. Their compulsivity does not interfere with task completion or promote
indecisiveness, nor do polio survivors lack generosity in giving to others. On the
contrary, compulsive behaviors are goal-oriented and are performed in the service of
others. Importantly, these behaviors are associated with the exacerbation and
maintenance of PPS symptoms. Because of these differences with OCPD, a separate
diagnostic category, Compulsive Psychophysiological Disorder (CPD), is suggested to
highlight the relationship between goal-oriented, compulsive behaviors and the
occurrence of physical symptoms (Table 3).
Fifty percent of the patients evaluated by this service met the criteria for CPD. Further,
the diagnosis of CPD is significantly correlated with patients' elevated Type A (r=.46)
and Sensitivity to Criticism and Failure scores (r=.47) suggesting that compulsive
behaviors are related to Type A behavior and may also serve in part to prevent criticism
and to protect against feelings of failure. These findings support the theoretical literature
on compulsive behavior, which suggests that compulsivity protects against loss of
control and failure (46) and is used to "avoid or overcome distressful feelings of
helplessness" (47)(see "flashbacks," below). Millon and Everly (48) state that
compulsive behavior occurs when the "child never develops a separate identity, and
functions in the world by conforming to strict, internalized parental standards and to the
standards around him or her" - conditions that are described above as central to the
experience of polio. And, compulsive behavior has been seen to develop in children
hospitalized even for brief periods (20).
Compulsive, Type A Behavior and the Etiology of PPS
Unfortunately, polio survivors appear to have paid a high price for learning compulsive,
Type A behavior in an effort to achieve "normalcy," escape "mortal danger" (15) and
protect against the emotional pain generated by the polio experience. That price is Post-
Polio Sequelae (28). Physical overexertion and emotional stress were reported to be the
first and second leading causes of PPS on the 1985 National Survey (5). The majority of
respondents to the 1990 National Survey reported symptoms of chronic stress (frequent
feelings of anxiety, low mood and difficulty falling asleep because the "mind is
racing")(6,7,8). These symptoms, along with the Type A and Sensitivity to Criticism
and Failure scores, were significantly correlated with PPS symptom severity (Table
2)(5,6,49).
These data indicate that PPS are psychophysiological in nature and that clinicians must
address both physical and psychological symptoms when polio survivors present for
treatment of PPS. Thus, the treatment of PPS requires behavior modification to reduce
compulsive, Type A behavior and thereby decrease PPS symptoms. Psychotherapy is
also necessary to address the dysfunctional beliefs and powerful suppressed emotions
resulting from the experience of polio that motivate compulsive, Type A behavior,
produce psychological distress and prevent compliance with therapy.
Behavioral Modification and Psychotherapy in Treating PPS
All patients who present for treatment by the Post-Polio Service undergo complete
physiatric and psychological evaluations, the latter beginning with administration of the
Reinforcement Motivation Survey (RMS) (43) and Beck Depression Inventory (BDI)
(50). Of the 32 patients evaluated during the past year, the majority had elevated Type
A (mean = 57 ± 28 ) and Sensitivity to Criticism and Failure (mean = 75 ± 28) scores on
the RMS but had insignificantly elevated BDI scores (mean = 14 ± 9).
Although 57% of patients reported "low mood," only 31% met DSM-IIIR criteria for
Major Depressive Episode (MDE), a percentage similar to the 32% reported by
Freidenberg, et al. (51) but higher than the prevalence of MDE in the general population
(3% to 7%) (52,53) and in those with medical illness (20%) (54). Friedenberg, et al.
(51) suggested that damage to monoaminergic neurons in the brain stem may predispose
polio survivors to MDE (see 49). However, the report of "treated depressions" in 38%
of adults with spina bifida suggests that childhood-onset orthopedic disability itself may
predispose to MDE in adults (55).
The presence of MDE in our patients is important, not only because it requires
treatment, but also because MDE is significantly correlated with treatment non-
compliance. MDE was diagnosed in 63% of patients who refused further treatment after
the initial evaluation and in 50% of those who were discharged for therapeutic non-
compliance. Only 11% of patients who were fully compliant and 29% of those who
were partially compliant with therapy were diagnosed as having a MDE. MDE is
always treated with psychotherapy, although depression was sufficiently severe in 70%
of patients that an antidepressant was recommended.
Following psychometric testing, psychological, medical and psycho social histories are
taken that include detailed descriptions of the new symptoms and their causes, the acute
polio experience, post-polio rehabilitation and patients' personal experience of
disability. Information about the response of family, friends and community to the acute
polio, to patients' original disability and to PPS is elicited along with a chronology of
school and vocational achievements noting the onset and development of compulsive,
Type A behavior.
Treatment. The treatment of PPS is approached by all members of the treatment team -
physician, psychologist and occupational and physical therapists - from a
psychophysiological perspective using the techniques of multimodal behavior therapy
(56). Therapy begins by asking patients to list their treatment goals and keep a daily log
of activities, perceived exertion, fatigue, muscle weakness, pain, emotional stress,
thoughts and emotions. This log is used to document physical and emotional symptoms
and demonstrate their relationship to thoughts, affect and compulsive, Type A behavior

(56). Outpatients are then evaluated by occupational and physical therapists during
twice-weekly sessions. Inpatients receive all therapies daily. After two weeks, log data
and evaluation results are used by the treatment team to formulate a behavioral plan
designed to decrease behaviors that cause physical symptoms, initiate self-care activities
and incorporate stress and time management, energy conservation, work simplification
and a program of relaxation, stretching and non-fatiguing progressive resistance
exercises (57) into patients' daily routine. The behavioral plan is then presented to
patients and their significant others at a meeting with the treatment team. Also discussed
are the hypothesized causes of PPS, the need to modify behavior to treat PPS and the
team's expectation of total compliance with all aspects of the behavioral plan. Patients
continue to keep logs throughout their treatment to document symptoms, the
progression of exercises and modification of behaviors. Logs are reviewed with patients
by each therapist at every treatment session. Goals are reviewed by the entire treatment
team at twice-monthly behavioral rounds. Problems with the behavioral plan, especially
those having to do with compliance, are communicated immediately to all members of
the team. Significant problems with compliance may require that patients be called in to
meet with the team. If no significant problems develop, patients meet with the team
once again at the end of the eight to twelve week treatment program.
Compliance problems often arise with the daily log and the behavioral plan. Patients
have difficulty keeping the log because it interferes with the compulsive performance of
their scheduled activities and forces them to recognize the severity and pervasiveness of
their symptoms. Invariably, patients have difficulty in complying with the behavioral
plan. They will 'forget' to alter their schedules and refuse lifestyle modification because
such changes directly conflict with their compulsive, Type A behavior (46). As one
patient who was discharged for non-complince angrily stated, "I don't want to change. I
just want to be the way I was."
Unfortunately, such problems with compliance are typical of post-polio patients. One
clinic reported that only 41% of patients sporadically used a newly prescribed brace
while 70% refused to use a new cane or crutch simply because they "didn't want to"
(58). Another clinic concluded that "the major reason for failure (of PPS symptoms) to
improve was the unwillingness of the patient to follow any of the recommendations
made" (59). Peach (60) has documented the importance of compliance with regard to
the treatment of PPS muscle weakness, showing that muscle strength decreases over
time only in patients who fail to fully comply with therapeutic recommendations.
During the past year, 47% of the patients treated by this service were judged to be fully
compliant, 34% only partially compliant while 19% were discharged from therapy for
not complying with the behavioral plan . Of all patients who received an initial
evaluation, 28% refused any treatment for their PPS. It appears that inadequate
compliance results in part from patients' fear of relinquishing compulsive, Type A
behavior that is believed by them to protect against "mortal danger" (15). Some non-
compliant patients fear that PPS will return them to the same position of helplessness
that they experienced following acute polio (cf. 47). Most report an even greater fear of
criticism and a sense of failure when they merely contemplate lifestyle changes or the
use of new assistive devices, even though without them PPS symptoms persist, progress
and functional ability deteriorates. Not unexpectedly, inadequately compliant patients
have an elevated mean Sensitivity to Criticism and Failure score (81 ± 2 0) as compared
to fully compliant patients (74 ± 35).
Patients' ability to change their behavior is directly related to their ability to challenge
long-held beliefs about self-worth and survival and tolerate the emergence of the
powerful fears and long-suppressed emotions generated by the polio experience (41). To
promote compliance with the behavioral plan, cognitive therapy techniques are
employed through weekly individual psychotherapy to identify and modify
dysfunctional beliefs, fears and emotions (46). Learning theory is also employed to
explain how compulsive, Type A behavior was learned to protect against fear,
emotional pain and "mortal danger" (15), while behavior modification techniques are
used to decrease and eliminate these overlearned behaviors (41,46).
As these techniques assist patients to decrease compulsive, Type A behavior, increased
anxiety and fear invariably result. Some patients report insomnia, panic attacks,
intrusive and emotionally-charged flashbacks about their early polio experience and
even fear of impending death (47). The psychotherapist then helps patients understand
the origin of these most disturbing experiences and learn to tolerate them, reinforces the
new self-care behaviors and supports patients through what can be terrifying days and
nights.
As therapy continues, patients discover that their compulsive, Type A behavior has been
more habitual than necessary. They begin to discard the "Good List," become better
able to care for themselves and begin to believe that they can have both self-worth and a
disability. As the behaviors and emotions conditioned by the polio experience decrease,
the focus of psychotherapy shifts to the experience of PPS. Depressed mood is replaced
by sadness and anger as the trauma of a "second disability" is experienced (4). Twice-
monthly group psychotherapy provides peer support to assist patients in dealing
emotionally with their PPS and practically with the lifestyle changes necessary to treat
them. The realization by patients in the group that they are not alone in their painful
physical and emotional experiences is itself powerfully therapeutic. Couples and family
sessions are also employed for both education about PPS and psychotherapy. It is
noteworthy that nearly all spouses, with some striking exceptions, respond favorably to
patients' lifestyle changes with the most frequently heard comment being, "I've been
wanting you to slow down for years."
All patients treated by this Service, whether fully or even partially compliant, report
meaningful reductions in physical and affective symptoms and increased function (cf.
60). But, as fatigue, muscle weakness and pain decrease, patients frequently increase
activity and have a tendency to resume compulsive, Type A behavior (46). To prevent
this, patients are instructed to strictly adhere to the modified daily schedule as set forth
in their behavioral plan, especially after they are discharged from physical and
occupational therapies and individual psychotherapy. Patients continue in group
psychotherapy for at least six months after discharge, are seen at three-month intervals
for medical and psychological follow-up and are encouraged to call their therapists at
any time with questions or for support.
Conclusion
It is possible that the large proportion of patients treated by this Service who have
experienced severe psychological trauma as a result of their polio experience may not
be representative of all polio survivors or even of all individuals who present for
treatment of PPS. However, there is something unique about the experience of polio that
predisposes to the development of compulsive, Type A behavior, sensitivity to criticism
and failure and chronic stress, anxiety and depression: the early onset of a universally
feared, potentially life-threatening illness that presented in epidemic proportions; the
experience of severe paralysis that could be forced to recede with the application of
years of strenuous physical therapy; the need to maximize physical abilities in order to
function in a "barrier-full" society that was repelled by disability; the sparing of
intellectual abilities that were used to overcompensate for residual physical limitations
(61,62). These factors must be studied if we are to understand the psychology of the
polio survivor, maximize treatment compliance and effectively treat both the physical
and psychological symptoms of PPS.
TABLES
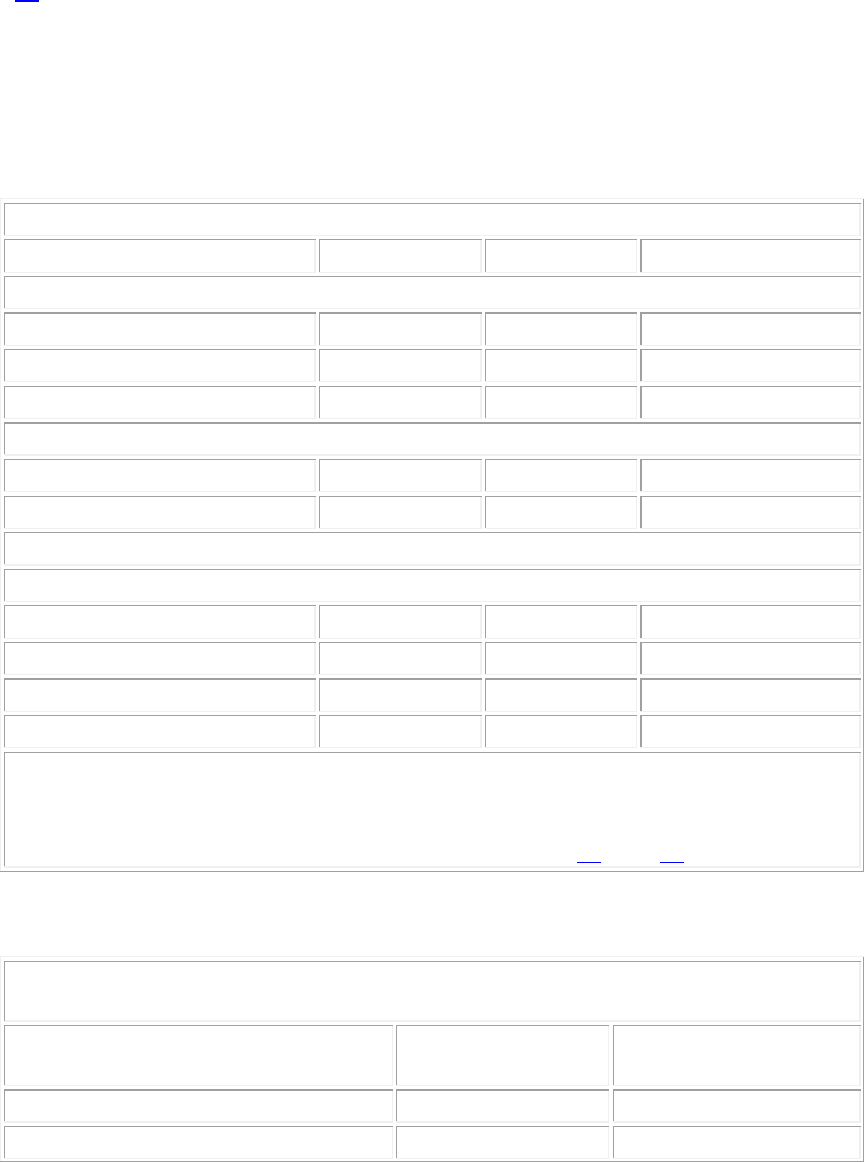
Table 1 [below]
EDUCATIONAL, MARITAL, AND EMPLOYMENT STATUS*
Post-Polio
Disabled
Non-Disabled
Marital Status
Single
11%
13%§
22%§
Married
71%
56%
58%
Other¤
18%
31%
20%
Education
< High school
29%
71%§
52%§
> High school
71%
29%
48%
Employment Status
Working
All positions¥
53%
38%§
79%**
Full time
40%
24%
59%
Unemployed
3%
62%
6%
Disability payments
28%
36%
1%
* Respondents to the 1990 National Post-Polio Survey compared with disabled and non-
disabled Americans.
¤ Divorced, widowed, or separated.
¥ Full-time, part-time, or homemaker. Data from reference 35§ and 36**.
Table 2 [below]
DEMOGRAPHIC DATA, NEW SYMPTOMS, AND PSYCHOLOGICAL
MEASURES*
Post-Polio Subjects
(n = 373)
Non-Disabled Controls
(n = 145)
Age
54 ( ±11 )¤
47 ( ± 14)
Female/Male ratio
1.5
1.5
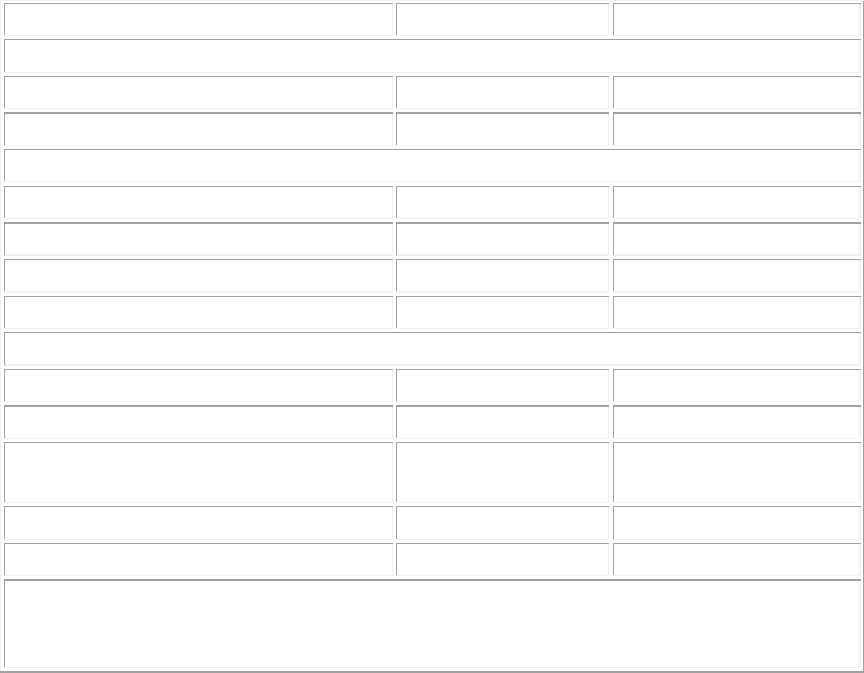
Years of education
14.5 ( ± 3)
15 ( ± 3)
Reinforcement Motivation Survey Scores:
Type A
59 ( ± 22)¤
45 ( ± 20)
Sensitivity to Criticism and Failure
68 ( ± 28)¤
59 ( ± 27)
New Symptoms
Fatigue
83%¥
15%
Muscle weakness
75%¥
9%
Pain
72%¥
15%
Emotional stress increases symptoms
75%¥
53%
Psychological Symptoms
Frequent feelings of anxiety
69%¥
36%
Chronic back/neck pain
66%¥
35%
Frequent trouble falling asleep
because "mind is racing"
65%¥
33%
Frequent "low mood"
57%§
41%
Diagnosed depression
27%§
15%
* From the 1990 National Post-Polio Survey
Significantly different from control values using independent groups t-test (¤P<.001) or
chi-square statistics (§P<.002; ¥P<.0001).
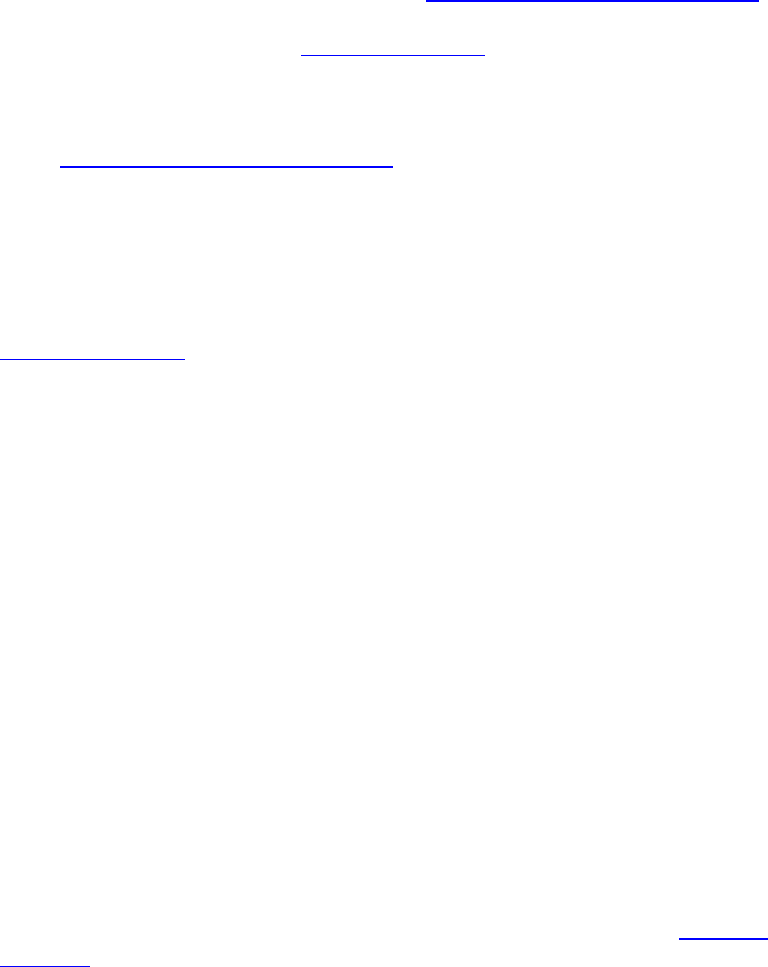
Table 3 [below]
DIAGNOSTIC CRITERIA FOR COMPULSIVE PSYCHOPHYSIOLOGICAL
DISORDER
A.
A pervasive pattern of continuous and excessive goal-oriented behaviour beginning
in childhood or adolescence as indicated by at least four of the following:
1.
Marked anxiety generated by and avoidance of any decrease in goal-oriented
activities or changes in daily schedule
2.
Refusal to delegate responsibilities or allow others to provide assistance
associated with an unusually strong need to be in control
3.
Rigidly and inflexibly judges behaviour on the basis of ideals of perfection or
"normality"
4.
Excessive time-consciousness and Type A behaviour
5.
Extreme sensitivity to criticism with the constant expectation of failure and
rejection
6.
Inability to identify or express emotion, with the exception of anxiety, anger, and
sadness.
B.
The association of these behaviours with the exacerbation or maintenance of physical
symptoms, such as muscle spasm-induced pain, fatigue, or muscle weakness.
REFERENCES
1. Gallagher HG: FDR's Splendid Deception. New York, Dodd, Mead, 1985.
2. Parsons PE: Data on polio survivors from the National Health Interview Survey.
Washington, D.C., National Center for Health Statistics, 1989.
3. Frick NM: Post-Polio Sequelae: Physiological and Psychological Overview.
Rehabilitation Literature 1986: 47:106-111. [Lincolnshire Library Full Text]
4. Frick NM: Post-Polio Sequelae and the psychology of second disability.
Orthopedics 1985; 8: 851-853. [PubMed Abstract]
5. Bruno RL, Frick NM: Stress and "Type A" behavior as precipitants of Post-
Polio Sequelae, in Halstead LS and Wiechers DO (eds): Research and CLinical
Aspects of the Late Effects of Poliomyelitis. White Plains, March of Dimes,
1987. [Lincolnshire Library Full Text]
6. Bruno RL, Frick NM: Psychological profile of polio survivors. Arch Phys Med
Rehabil 1990; 10: 889.
7. Bruno RL, Frick NM: Five year follow-up to the 1985 National Post-Polio
Survey. Arch Phys Med Rehabil 1990; 10: 886.
8. Conrady LJ, Wish JR, Agre JC, Rodriquez, AA, Sperling, KB: Psychological
characteristics of polio survivors. Arch Phys Med Rehabil 1989; 70: 458-463.
[PubMed Abstract]
9. Bozarth CH: Unfinished Business: Support Group Members Confront Feelings
Surrounding the Late Effects of Polio. Lansing, Polio Survivors Support Group,
1987.
10. Copellman FS: Follow-up of one hundred children with poliomyelitis. The
Family 1944; December: 189-196.
11. Meyer E: Psychological considerations in a group of children with
poliomyelitis. J Pediatrics 1947; 31: 34-48.
12. Moustakas CE: Loneliness. Englewood Cliffs, Prentice Hall, 1961.
13. Seidenfeld MA: The psychological sequelae of poliomyelitis in children. The
Nervous Child 1948; 7: 14-28.
14. Wright BA: Physical Disability - A psychosocial approach. New York, Harper
and Row, 1983.
15. Register C: Living with Chronic Illness. New York, Free Press, 1987.
16. Berg RH: Polio and its Problems. Philadelphia, Lippincott, 1948.
17. Billig HE, van Harreveld A, Wiersma CAG: On re-innervation of paretic
muscles by the use of their residual nerve supply. J Neuropath Exp Neurol 1946;
5:1-23.
18. Kerr N: Staff expectations for disabled persons. Rehabilitation Counseling
Bulletin 1970; 14: 85-94.
19. Hawke WA, Auerbach A: Multidiscipline experience: A fresh approach to aid
the multihandicapped child. Journal of Rehabilitation 1975: 41:22-24. [PubMed
Abstract]
20. Rowlands P: Children Apart. New York, Pantheon, 1973.
21. Schechter MD: The orthopedically handicapped child. Arch Gen Psychiatry
1961; 4: 53-59.
22. Davis F: Passage Through Crisis. Indianapolis, Bobbs-Merrill,1963.
23. Rice EP: The families of children with poliomyelitis, in Poliomyelitis.
Philadelphia, Lippincott, 1949.
24. Moustakas CE: Loneliness and Love. Englewood Cliffs, Prentice Hall, 1972.
25. Ladieu-Leviton G, Adler DL, Dembo T: Studies in adjustment to visible
injuries: Social acceptance of the injured. Journal of Social Issues 1948; 4: 55-
62.
26. Davis F: Illness, Interaction and the Self. Belmont, California, Wadsworth,
1972.
27. Long L, Roth C: The psychological aspects of rehabilitation, in Soden WH (ed)
Rehabilitation of the Handicapped. New York, Ronald, 1949.
28. Trieschmann RB: Aging with a Disability. New York, Demos, 1987.
29. Battle CU: Disruptions in the socialization of a young, severely handicapped
child. Rehabilitation Literature 1974; 35:130-140. [PubMed Abstract]
30. Anthony WA: Societal rehabilitation: Changing society's attitudes toward the
physically and mentally disabled. Rehabilitation Psychology 1972; 19: 117-126.
31. Wright BA: Issues in overcoming emotional barriers to adjustment in the
handicapped. Rehabilitation Counseling Bulletin 1967; 11: 53-59.
32. Bloom JL: Sex education for the physically handicapped. Sexology 1970; 36:
62-65.
33. Hohmann GW: Reactions of the individual with a disability complicated by a
sexual problem. Arch Phys Med Rehabil 1975; 56: 8-13. [PubMed Abstract]
34. Ladieu G, Hanfmann E, Dembo T: Studies in adjustment to visible disability.
The Journal of Abnormal Social Psychology 1947; 42: 169-192.
35. Taylor H, Kagay MR, Leichenko S: The ICD Survey of Disabled Americans.
New York, Louis Harris, 1986.
36. Statistical Abstract of the United States: 1990 (110th edition). U.S. Bureau of
the Census, Washington, D.C., 1990.
37. Bruno RL, Frick NM: The origins of "Type A" behavior and stress induced
symptoms in polio survivors. Proceedings of the Society of Behavioral Medicine
1989; 10: 85.
38. Perkins KA: Heart rate change in Type A and Type B males as a function of
response cost and task difficulty. Psychophysiology 1984; 21: 14-21. [PubMed
Abstract]
39. Rosenman RH, Friedman M, Straus R, et al: A predictive study of coronary
heart disease. JAMA 1964; 189: 113-124.
40. Friedman M, Thoresen CE, Gill JJ, et al: Feasibility of altering Type A behavior
pattern. Circulation 1982; 66: 83-92. [PubMed Abstract]
41. Powell LH, Friedman M, Thoresen CE, et al: Can the Type A behavior pattern
be altered after myocardial infarction? Psychosom Med 1984; 46: 293-313.
[PubMed Abstract]
42. Young LD, Barboriak JJ: Reliability of a brief scale for assessment of coronary-
prone behavior and standard measures of Type A behavior. Percept Mot Skills
1982; 55: 1039-1042. [PubMed Abstract]
43. Bruno RL: Predicting pain management program outcome: The Reinforcement
Motivation Survey. Arch Phys Med Rehabil 1990; 10: 785.
44. Mandell AJ: Toward a psychobiology of transcendence, in Davidson JM,
Davidson RJ (eds): The Psychobiology of Consciousness, New York, Plenum, 1
980.
45. Diagnostic and Statistical Manual of Mental Disorders (ed 3, revised).
Washington, D.C., American Psychiatric Association, 1987.
46. Beck AT, Freeman A: Cognitive Therapy of Personality Disorders. New York,
Guilford, 1990.
47. Salzman L: The Obsessive Personality. New York, Jason Aronson, 1973.
48. Millon T, Everly G: Personality and its Disorders. New York, Wiley, 1985.
49. Bruno RL, Frick NM, Cohen J. Polioencephalitis, stress and the etiology of
Post-Polio Sequelae. Orthopedics 1991; (this issue). [Lincolnshire Library
Full Text]
50. Beck AT, Ward CH, Mendelson M, et al: An inventory for measuring
depression. Arch Gen Psychiatry 1961; 4: 561-571.
51. Freidenberg DL, Freeman D, Huber SJ, Perry, J, Fischer, A, Van Gorp, W G, et
al: Postpoliomyelitis Syndrome: Behavioral Features. Neuropsychiatry,
Neuropsychology and Behavioral Neurology 1989; 2: 272-281. [Lincolnshire
Library Full Text]
52. Myers JK, Weissman MM, Tischler OL, et al: Six month prevalence of
psychiatric disorders in three communities. Arch Gen Psychiatry 1984; 41: 959-
967. [PubMed Abstract]
53. Roberts RE, Vernon SW: Depression in the community: Prevalence and
treatment. Arch Gen Psychiatry 1982; 39: 1407-1409. [PubMed Abstract]
54. Schleifer SJ, Macari M, Slater W, et al: Predictors of outcome after myocardial
infarction: Role of depression. Circulation 1987; 74 (supplement II): 38.
55. Dunne KB, Gingher N, Olsen L, et al: The Adult Spina Bifida Network Survey.
Insights 1986; 14: 28-32.
56. Lazarus A: Multimodal Behavior Therapy. New York, Springer Verlag, 1976.
57. Fillyaw, et al. Orthopedics December, 1991.
58. Waring WP, Maynard F, Grady W et al: Influence of appropirate lower
extremity orthotic management on ambulation, pain and fatigue in a postpolio
population. Arch Phys Med Rehabil 1989; 70: 371-375. [PubMed Abstract]
59. Agre JC, Rodriquez AA, Sperling KB: Symptoms and clinical impressions of
patients seen in a postpolio clinic. Arch Phys Med Rehabil 1989; 70: 367-370.
[PubMed Abstract]
60. Peach PE, Olejnik S: Effects of treatment and noncompliance on post-polio
sequelae symptoms and muscle strength. Orthopedics 1991; (this issue).
[Lincolnshire Library Full Text]
61. Scheer J, Luborsky M: Culture and polio. Orthopedics 1991; (this issue).
[PubMed Abstract]
62. Not present in source document.
